Blog
How Diabetes Can Affect Your Feet

Diabetes can cause serious problems for your feet if not managed well. High blood sugar levels can damage the nerves in your feet, leading to numbness, tingling, or loss of feeling, which is called diabetic neuropathy. When you cannot feel pain, you might not notice cuts, blisters, or sores. Diabetes can also slow down blood flow, making it harder for wounds to heal and increasing the risk of infection. If infections are not treated quickly, they can lead to serious complications, including loss of limbs. Daily foot care is important for people with diabetes. Check your feet every day for cuts, redness, or swelling, and wear shoes that protect your feet. If you have diabetes, it is suggested that you see a podiatrist regularly for help in addressing problems early and keeping your feet healthy.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Soothing Aching Feet With Simple Exercises

Achy feet can result from long hours of standing, walking, or wearing unsupportive footwear. Stretching helps relieve tension by loosening tight muscles and improving flexibility. Simple stretches, such as pulling the toes back gently or rolling the foot over a massage ball, can provide relief. The marble pick-up exercise strengthens the toes and arches by encouraging small muscle activation. Drawing the alphabet with the ankle helps improve mobility and reduce stiffness by engaging the entire foot and lower leg. Calf raises strengthen the lower legs and improve circulation, which can reduce swelling and fatigue. Incorporating these exercises into a daily routine can relieve discomfort, improve foot strength, and enhance overall foot health. If your feet ache the majority of the time, it is suggested that you consult a podiatrist who can guide you on effective relief tips, which may include additional foot stretches.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Facts About Toenail Fungus

Toenail fungus, medically known as onychomycosis, causes discoloration, thickening, and in advanced cases, crumbling of the toenail. Fungal infections thrive in warm, damp environments, making places like swimming pool areas, gym locker rooms, and moist footwear ideal for growth. Symptoms of toenail fungus include nails turning yellow, brown, or green, as well as thickened nails that may become brittle or distorted. A podiatrist can effectively diagnose and manage toenail fungus through prescription antifungal medications or, in severe instances, surgery to remove the infected nail. Early intervention is important to avoid the infection spreading to adjacent toenails or to other people. Patients with diabetes should be especially vigilant because fungal nail infections can lead to sores or complications due to impaired circulation and healing. If you suspect you have a fungal toenail infection, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and treatment.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact one of our podiatrists of James Kutchback, DPM, CWS-P. Our doctors can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions please contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
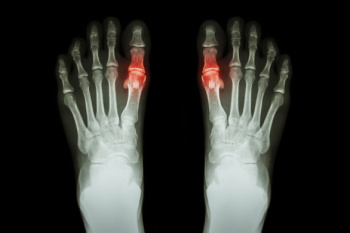
Understanding Bunions

Bunions are bony bumps that form at the base of the big toe, often caused when the tip of the toe angles inward toward the other toes. This deformity can lead to pain, swelling, redness, and difficulty finding comfortable shoes. The affected area may become tender, and, as the bunion progresses, it can affect walking and lead to other foot issues like calluses or hammertoes. A podiatrist can evaluate your bunion and offer various treatments. For mild cases, they may recommend lifestyle changes, such as wearing shoes with a wider toe box or using padding to reduce pressure. Custom orthotics can help correct foot alignment, providing relief from discomfort. In more severe cases, a podiatrist may suggest surgical options to correct the deformity and improve function. If you are experiencing pain or discomfort from a bunion, it is suggested that you schedule an appointment with a podiatrist.
If you are suffering from bunions, contact one of our podiatrists of James Kutchback, DPM, CWS-P. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Neuropathy and the Feet

Peripheral neuropathy is a condition that affects the nerves in the feet, toes, and ankles, leading to symptoms such as burning, tingling, numbness, and pain. These symptoms can make it difficult to feel injuries or changes in temperature, which increases the risk of developing blisters, sores, and infections. Over time, untreated infections may lead to serious complications, including changes in foot structure or, in severe cases, the loss of a toe or foot. People with peripheral neuropathy may also experience muscle weakness and balance problems, making them more prone to falls. A podiatrist plays a key role in managing peripheral neuropathy by performing detailed exams to assess nerve function and blood flow in the feet. Monofilament exams and tuning fork evaluations can help determine the extent of nerve damage. A podiatrist can also provide guidance on proper foot care, early treatment for injuries, and strategies to prevent complications. If you have symptoms of peripheral neuropathy that affect your feet, it is suggested that you make an appointment with a podiatrist for an exam and treatment options.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Definition and Risk Factors of Heel Spurs
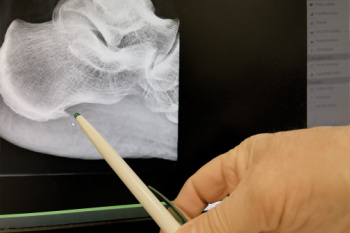
A heel spur is a bony growth that forms on the underside of the heel bone, often as a result of prolonged strain and pressure on the foot. This condition is commonly associated with plantar fasciitis, an inflammation of the tissue along the bottom of the foot. The main symptom of a heel spur is sharp pain at the bottom of the heel, particularly when standing up after a period of rest, such as first thing in the morning. The pain can also worsen after prolonged periods of standing or walking. Risk factors for developing heel spurs include being overweight, having flat feet or high arches, and wearing improper footwear. Also, engaging in activities that put excessive strain on the feet, such as running or standing for long periods of time may lead to developing a heel spur. Age and certain medical conditions, like diabetes, can increase the likelihood of developing heel spurs as well. If you have heel pain, it is suggested that you consult a podiatrist who can provide an accurate diagnosis and treatment.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Managing Gout
Gout is a type of arthritis caused by the buildup of uric acid crystals in the joints, often affecting the big toe. It occurs when the body produces too much uric acid or does not excrete enough through urine. Symptoms include sudden, intense pain, redness, swelling, and warmth in the affected joint, typically during the night. Gout attacks can feel excruciating, making even the lightest touch unbearable. Treatment for gout involves medications like nonsteroidal anti-inflammatory drugs called NSAIDs, colchicine, or corticosteroids to reduce pain and inflammation. Long-term management may include medications to lower uric acid levels and lifestyle changes like reducing alcohol intake and eating a purine-free diet. A podiatrist can help diagnose gout, manage flare-ups, and provide advice on footwear and exercises to reduce strain on affected joints. If you are experiencing symptoms of gout, it is suggested that you schedle an appointment with a podiatrist for effective treatment and management.
Gout is a painful condition that can be treated. If you are seeking treatment, contact one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors will treat your foot and ankle needs.
What Is Gout?
Gout is a form of arthritis that is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. The condition usually affects the joint at the base of the big toe. A gout attack can occur at any random time, such as the middle of the night while you are asleep.
Symptoms
- Intense Joint Pain - Usually around the large joint of your big toe, and it most severe within the first four to twelve hours
- Lingering Discomfort - Joint discomfort may last from a few days to a few weeks
- Inflammation and Redness -Affected joints may become swollen, tender, warm and red
- Limited Range of Motion - May experience a decrease in joint mobility
Risk Factors
- Genetics - If family members have gout, you’re more likely to have it
- Medications - Diuretic medications can raise uric acid levels
- Gender/Age - Gout is more common in men until the age of 60. It is believed that estrogen protects women until that point
- Diet - Eating red meat and shellfish increases your risk
- Alcohol - Having more than two alcoholic drinks per day increases your risk
- Obesity - Obese people are at a higher risk for gout
Prior to visiting your podiatrist to receive treatment for gout, there are a few things you should do beforehand. If you have gout you should write down your symptoms--including when they started and how often you experience them, important medical information you may have, and any questions you may have. Writing down these three things will help your podiatrist in assessing your specific situation so that he or she may provide the best route of treatment for you.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Managing Athlete’s Foot

Athlete's foot is a fungal infection that affects the skin on your feet, often between the toes, however, there is also a moccasin variety that affects the bottom of the feet. It is caused by dermatophytes, fungi that thrive in warm, moist environments, such as sweaty shoes or locker rooms. The condition is highly contagious and can spread through direct contact with infected surfaces or people. Common symptoms of athlete's foot include itching, burning, peeling, and redness. In more severe cases, the skin may crack, blister, or become painful. It can also spread to the toenails or other areas of the body if left untreated. Treatment typically involves antifungal creams or powders, which help eliminate the infection. Keeping your feet dry and wearing breathable shoes are also key to preventing reinfection. In stubborn cases, a podiatrist may prescribe stronger antifungal medications or recommend a more tailored treatment plan. If you are experiencing symptoms of athlete's foot, it is suggested that you schedule an appointment with a podiatrist for proper diagnosis and treatment.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.