Items filtered by date: July 2020
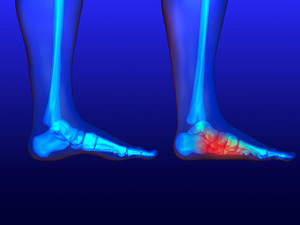
Flatfoot
Flatfoot is a foot disorder that is not as straightforward as many people believe. Various types of flatfoot exist, each with their own varying deformities and symptoms. The partial or total collapse of the arch, however, is a characteristic common to all types of flatfoot. Other signs of flatfoot include:
- “Toe drift,” or the pointing outward of the toes and the front part of the foot
- The tilting outward of the heel and the tilting inward of the ankle
- The lifting of the heel off the ground earlier when walking due to a tight Achilles tendon
- Hammertoes
- Bunions
One of the most common types of flatfoot is flexible flatfoot. This variation usually starts in childhood and progresses as one ages into adulthood. Flexible flatfoot presents as a foot that is flat when standing, or weight-bearing. When not standing, the arch returns. Symptoms of flexible flatfoot include:
- Pain located in the heel, arch, ankle, or along the outside of the foot
- Overpronation, or an ankle that rolls in
- Shin splint, or pain along the shin bone
- General foot aches or fatigue
- Pain located in the lower back, hip, or knee
Your podiatrist will most likely diagnose flatfoot by examining your feet when you stand and sit. X-rays may be taken to define the severity and help determine the treatment option best for your condition. Nonsurgical treatments can include activity modification, weight loss, orthotics, immobilization, medications, physical therapy, shoe modifications, and ankle foot orthoses (AFO) devices. If nonsurgical methods prove ineffective, surgery may be considered. Multiple surgical procedures can correct flatfoot; and depending on your specific condition, one may be selected alone or combined with other techniques to ensure optimal results.
How to Determine If I Have Flat Feet
 The condition that is known as flat feet can be noticeable while standing on the floor. The arch area of the feet will lie flat on the floor, and the feet may feel achy. The majority of babies are born with flat feet, and the arch typically develops throughout childhood. The arch provides flexibility between the front and back of the foot, in addition to dispersing body weight while standing up. Many patients with flat feet choose to wear custom made orthotics, and this may help to provide mild relief with additional cushioning. If you have pain in your feet and think you may have flat feet, it is suggested that you consult with a podiatrist who can properly diagnose you and offer treatment options.
The condition that is known as flat feet can be noticeable while standing on the floor. The arch area of the feet will lie flat on the floor, and the feet may feel achy. The majority of babies are born with flat feet, and the arch typically develops throughout childhood. The arch provides flexibility between the front and back of the foot, in addition to dispersing body weight while standing up. Many patients with flat feet choose to wear custom made orthotics, and this may help to provide mild relief with additional cushioning. If you have pain in your feet and think you may have flat feet, it is suggested that you consult with a podiatrist who can properly diagnose you and offer treatment options.
Flatfoot is a condition many people suffer from. If you have flat feet, contact one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
Our feet are arguably the most important parts of our bodies because they are responsible for getting us from place to place. However, we often don’t think about our feet until they begin to hurt. If you have pain in your feet, you need to first determine where on the foot you are experiencing it to get to the root of the problem. The most common areas to feel pain on the foot are the heel and the ankle.
Heel pain is most commonly attributed to a condition called plantar fasciitis. Plantar fasciitis occurs when the plantar fascia, which is the band of tough tissue connecting the heel bone to the toes becomes inflamed. Plantar fasciitis pain is usually worse in the morning, and it tends to go away throughout the day. If you have plantar fasciitis, you should rest your foot and do heel and foot muscles stretches. Wearing shoes with proper arch support and a cushioned sole has also been proven to be beneficial.
Some common symptoms of foot pain are redness, swelling, and stiffness. Foot pain can be dull or sharp depending on its underlying cause. Toe pain can also occur, and it is usually caused by gout, bunions, hammertoes, ingrown toenails, sprains, fractures, and corns.
If you have severe pain in your feet, you should immediately seek assistance from your podiatrist for treatment. Depending on the cause of your pain, your podiatrist may give you a variety of treatment options.
Types of Foot Pain
 Each foot consists of twenty six bones, numerous ligaments, muscles, and tendons. Everyday wear and tear or an injury can compromise general foot function, and uncomfortable foot conditions may occur. A bunion is a bony formation that develops on the side of the big toe, and can happen from wearing shoes that do not fit correctly. Blisters can occur on the back of the heel or on the bottom of the feet, and this is generally a result of increased friction. A corn is a hardened area that can gradually develop on top of the toes or between them, and can cause severe pain and discomfort. If you have these or other conditions that can lead to chronic foot pain, it is strongly advised that you are under the care of a podiatrist who can guide you toward proper treatment techniques.
Each foot consists of twenty six bones, numerous ligaments, muscles, and tendons. Everyday wear and tear or an injury can compromise general foot function, and uncomfortable foot conditions may occur. A bunion is a bony formation that develops on the side of the big toe, and can happen from wearing shoes that do not fit correctly. Blisters can occur on the back of the heel or on the bottom of the feet, and this is generally a result of increased friction. A corn is a hardened area that can gradually develop on top of the toes or between them, and can cause severe pain and discomfort. If you have these or other conditions that can lead to chronic foot pain, it is strongly advised that you are under the care of a podiatrist who can guide you toward proper treatment techniques.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels may make you want to think twice about showing off your feet in warmer weather. However, cracked heels may be harmful to more than just the appearance of your feet. If deep fissures and cracks develop in your heels, they may make walking and standing painful for you. Additionally, these openings make way for germs to enter through your skin and cause infection.
There are several different causes of cracked heels. One of the most common reasons for this ailment is dry skin. This problem may make your keeps feel rough tight and itchy. Dry skin may be caused by cold air, extremely hot water, harsh soaps, and aging. Skin disorders such as eczema and psoriasis may eventually lead to dry skin. In some cases, complications may arise from cracked heels. Some of these complications are a loss of feeling in the heel, cellulitis, or a diabetic foot ulcer.
There are ways you can try to prevent getting cracked heels. One of the best ways to do so is to avoid wearing flip flops and sandals because these shoes increase your risk of drying out your feet. You should also avoid wearing shoes with a tall skinny heel, because these shoes cause your heel to expand sideways. At night, you should slather on a thick moisturizing cream on your feet and then cover them in socks to keep your feet moisturized overnight. Drinking water to stay hydrated is also a good way to ensure that your skin doesn’t become dry.
If you suffer from a severe case of cracked feet, you should make an appointment with your podiatrist to see what treatment methods are best for you.
Causes of Cracked Heels
 Cracked heels or heel fissures are a common foot condition that can cause discomfort and sometimes pain. The first sign of cracked heels is having areas of dry, thickened skin, known as calluses, around the rim of your heel. As you walk the fat pad under your heel expands, causing the calluses to crack. Some factors for cracked heels to develop can be weight gain or obesity, standing on hard surfaces for extended periods of time, and open back shoes that do not provide adequate support for the heel of the foot. Most of the time cracked heels don't really hurt, but as the cracks deepen, they may bleed or cause standing and walking to become painful. To prevent cracked heels, it is recommended to apply a good moisturizer to the feet daily. Patients with diabetes should check their feet regularly, if the fissures go unnoticed, they could turn into diabetic foot ulcers. If your cracked heels are severe, it is suggested that you seek the counsel of a podiatrist who can guide you towards correct treatment options.
Cracked heels or heel fissures are a common foot condition that can cause discomfort and sometimes pain. The first sign of cracked heels is having areas of dry, thickened skin, known as calluses, around the rim of your heel. As you walk the fat pad under your heel expands, causing the calluses to crack. Some factors for cracked heels to develop can be weight gain or obesity, standing on hard surfaces for extended periods of time, and open back shoes that do not provide adequate support for the heel of the foot. Most of the time cracked heels don't really hurt, but as the cracks deepen, they may bleed or cause standing and walking to become painful. To prevent cracked heels, it is recommended to apply a good moisturizer to the feet daily. Patients with diabetes should check their feet regularly, if the fissures go unnoticed, they could turn into diabetic foot ulcers. If your cracked heels are severe, it is suggested that you seek the counsel of a podiatrist who can guide you towards correct treatment options.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Heel Pain And Plantar Fasciitis
There is a portion of tissue that is located on the bottom of the foot that is referred to as the plantar fascia. This part of the foot can gradually become damaged from standing on hard surfaces for the majority of the day, in addition to wearing shoes that do not fit correctly. This can cause plantar fasciitis, which is an inflammation of this band of tissue. A common symptom that many patients experience is heel pain, and this can cause difficulty in walking. The pain may be worse in the morning after arising, and may lessen during the day. People who are overweight may be prone to developing plantar fasciitis, in addition to people who have flat feet. Mild relief may be found when the feet are elevated, and it may be helpful to practice specific foot stretches. If you are afflicted with plantar fasciitis, it is advised that you are under the care of a podiatrist who can help you with correct treatment options.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.