Flipping Out About Flip Flops
Although it may be tempting to wear flip-flops in warm weather, they are not the best choice of footwear for your feet. Flip-flops may be ideal for the beach, pool, spa, and shared showers, but you should avoid wearing them unless it is completely necessary.
Flip-flops only have a small strip of fabric holding your foot in place, but your toes need a better grip to keep your foot in place. The repetitive gripping can lead to an overuse of your muscles, which could result in tendinitis. This is only one of the many problems that stem from wearing flip-flops too often.
Flip flops aren’t good for extensive walking because they fail to offer arch support, heel cushioning, or shock absorption. As a result, people who wear flip flops are at a higher risk of experiencing an ankle sprain. Additionally, these shoes offer little protection for your feet, putting those who wear them at a greater risk for stubbed toes, glass cuts, and puncture wounds.
Although flip flops aren’t recommended for everyday use by anyone, it is especially important for diabetics to avoid them. A diabetic foot injury can easily become very serious, and it may even lead to amputation.
If you are experiencing pain from wearing flip-flops, you shouldn’t be hesitant to replace them with a more comfortable shoe that offers more support. If your flip-flop foot pain doesn’t go away, you should seek assistance from a podiatrist right away. It is possible that you may have a more serious foot problem such as a stress fracture or arthritis.
What Are the Reasons for Stress Fractures to Develop?
 The most common reason for a stress fracture to develop is from overuse and participating in repetitive activities. Sporting events that require frequent running and jumping may cause stress fractures to gradually occur and this may cause pain and discomfort. Many patients may feel mild symptoms immediately following this type of injury and choose to ignore them. This can cause the stress fracture to worsen and the symptoms to intensify. People may also find if they increase the speed and duration of their training too quickly, a stress fracture may result from not gradually increasing speed and distance. Additionally, this type of ailment may occur from an abnormal foot structure or from wearing shoes that do not fit properly. If you incur this type of injury, it is suggested that you confer with a podiatrist when signs and symptoms first arise as there are several treatment options available.
The most common reason for a stress fracture to develop is from overuse and participating in repetitive activities. Sporting events that require frequent running and jumping may cause stress fractures to gradually occur and this may cause pain and discomfort. Many patients may feel mild symptoms immediately following this type of injury and choose to ignore them. This can cause the stress fracture to worsen and the symptoms to intensify. People may also find if they increase the speed and duration of their training too quickly, a stress fracture may result from not gradually increasing speed and distance. Additionally, this type of ailment may occur from an abnormal foot structure or from wearing shoes that do not fit properly. If you incur this type of injury, it is suggested that you confer with a podiatrist when signs and symptoms first arise as there are several treatment options available.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures are small breaks in the bone that are caused by repetitive stress. They typically occur due to overuse, forcing the bones of the foot or ankle to continually absorb the full impact of each step taken. Stress fractures can also be caused by abnormal foot structure, osteoporosis, bone deformities, or wearing improper footwear during exercise.
Stress fractures are common for individuals whose daily activities cause high levels of impact on their feet and ankles. Those who run, play tennis or basketball, or practice gymnastics tend to experience these fractures more frequently. Anyone is susceptible to this problem, though. Individuals who are normally sedentary and suddenly begin an intense, high impact workout may sustain stress fractures. This is because their muscles are not yet strong enough to handle and cushion the intensity of their activity. Osteoporosis may also cause someone to get stress fractures, because the disease weakens an afflicted person's bones and makes it easier for them to break down.
Pain from stress fractures typically occurs in the general area of the fracture. Pain can also manifest as “pinpoint pain” or pain that is felt when the site of the injury is touched, and can be accompanied by swelling. It may occur during or after activity, and it may disappear while resting and return when standing or moving. Engaging in any kind of activity, high impact or otherwise, will aggravate the pain. If the intensity of the activity increases before the stress fracture has properly healed, it can cause a full fracture.
Treatment can vary depending on the individual and the degree of injury. The primary way to treat a stress fracture is to rest the hurt foot. Some fractures will heal quickly with only a little bit of rest, while others may require a long rest period and the use of crutches, immobilization, or physical therapy. Under certain circumstances, surgery may be required to install support pins around the fracture to assist in healing.
If you are undergoing a new exercise regimen in running or some other kind of high impact activity, set incremental goals on a weekly basis so you can build up muscle strength. Make sure to wear supportive shoes to better protect you feet.
If you begin to experience any symptoms of stress fractures, you should stop exercising and rest. If the symptoms persist, consult with your podiatrist. Remembering these tips can help you prevent stress fractures to your foot and ankle, and allow you to continue living normally.
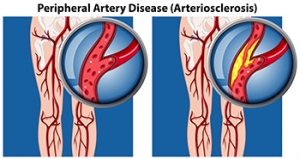
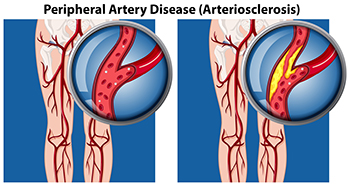
How Peripheral Arterial Disease Affects the Feet
Peripheral arterial disease (PAD) occurs when the outer, or peripheral, arteries narrow due to a build-up of plaque. Peripheral arteries transport blood—which carries oxygen and nutrients—to the legs and arms, keeping the skin and underlying tissue alive and healthy. When PAD is present in the legs, it can reduce the normal amount of blood flow, oxygen, and nutrients to the feet. This may lead to dysfunction in the skin and tissue, causing it to break down and make it more susceptible to developing wounds. PAD can be an inherited disease, or may be caused by diabetes, hypertension, high cholesterol, or obesity. Symptoms of PAD in the feet may include burning, aching, coolness, redness, reoccurring infections, and sores in the toes and feet that do not heal. If you are experiencing any of these symptoms, contact a podiatrist for a full examination, testing, diagnosis and proper treatment.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Why Aging Feet Need Regular Care
 Foot care for the elderly is important as skin tends to thin out and lose elasticity, and nails can become dry and brittle—making the feet more susceptible to infections, blisters, toenail fungus, ingrown toenails, and more. It is important for an aging adult to practice regular foot care, or if they cannot do it themselves, have a caretaker do it. Toenails should be trimmed and filed regularly: straight across, and not too short in order to avoid ingrown toenails. Nail clippers should be sanitized and never shared. Feet should be cleaned, moisturized, and inspected daily for signs of infection which may include cracks, blisters, discolored nails, or bleeding sores. Footwear should be properly sized with good arch support to aid in mobility and prevent slips and falls. Shoes should never force the feet or toes into a position that is uncomfortable or restricts circulation. Additionally, older adults should make an appointment with a podiatrist for an examination and possibly even a gait analysis to detect and treat any developing or existing conditions.
Foot care for the elderly is important as skin tends to thin out and lose elasticity, and nails can become dry and brittle—making the feet more susceptible to infections, blisters, toenail fungus, ingrown toenails, and more. It is important for an aging adult to practice regular foot care, or if they cannot do it themselves, have a caretaker do it. Toenails should be trimmed and filed regularly: straight across, and not too short in order to avoid ingrown toenails. Nail clippers should be sanitized and never shared. Feet should be cleaned, moisturized, and inspected daily for signs of infection which may include cracks, blisters, discolored nails, or bleeding sores. Footwear should be properly sized with good arch support to aid in mobility and prevent slips and falls. Shoes should never force the feet or toes into a position that is uncomfortable or restricts circulation. Additionally, older adults should make an appointment with a podiatrist for an examination and possibly even a gait analysis to detect and treat any developing or existing conditions.
Everyday foot care is very important to prevent infection and other foot ailments. If you need your feet checked, contact one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors can provide the care you need to keep you pain-free and on your feet.
Everyday Foot Care
Often, people take care of their bodies, face and hair more so than they do for their feet. But the feet are a very important aspect of our bodies, and one that we should pay more attention to. Without our feet, we would not be able to perform most daily tasks.
It is best to check your feet regularly to make sure there are no new bruises or cuts that you may not have noticed before. For dry feet, moisturizer can easily be a remedy and can be applied as often as necessary to the affected areas. Wearing shoes that fit well can also help you maintain good foot health, as well as making it easier to walk and do daily activities without the stress or pain of ill-fitting shoes, high heels, or even flip flops. Wearing clean socks with closed shoes is important to ensure that sweat and bacteria do not accumulate within the shoe. Clean socks help to prevent Athlete’s foot, fungi problems, bad odors, and can absorb sweat.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Everyday Foot Care
Our feet are arguably one of the most important parts of the body. When it comes to health and beauty routines, the feet and toenails are usually ignored. You should always practice proper footcare to avoid any fungal infections or ailments that can not only ruin the appearance of your feet, but also cause pain. Ignoring any foot problems could potentially lead to an expensive doctor’s visit.
The most important step in proper foot care is to wash your feet daily. You should wash them with soap and water. Doing this will cleanse your feet of dirt, sweat and bacteria. It is crucial that you clean between the toes and pat your feet dry with a towel afterward. Your toenails are also an important part of the feet and you may find that they get dirtier in the summer when you wear sandals. It is important that you practice proper toenail care in addition to cleaning the rest of your feet. When trimming your nails, you should always trim straight across instead of in a rounded shape. Trimming in a curved shape may lead to ingrown toenails.
Moisturization is also important for foot care, and you should be moisturizing your feet every day. The best way to prevent dry feet is to rub lotion or petroleum jelly on your clean feet at night and put socks over them. In the morning, your feet should be soft and moisturized.
Another crucial step in proper foot care is to wear the right shoes for whichever activity you are going to partake in. In warmer weather, you should wear shoes that allow your feet to breathe. It is best to avoid shoes such as flip-fops that do not provide arch support. Tight shoes may also be harmful, and they may even cause you to develop bunions.
If you plan on taking a shower in a public area, you should be especially careful, so you do not pick up any fungi. Showers are prone to harboring different types of bacteria and fungi. You should always wear shower shoes or flip flops when walking around in locker rooms and public showers. Avoid sharing shoes with other people because this is another way that fungus may be spread.
If you are experiencing any problems with your feet you should speak with your podiatrist to determine the best method of treatment for you.
Treatment For Diabetic Foot Ulcers
 Diabetic foot ulcers (DFUs) are slow-healing wounds that often form on the feet of people who have diabetes. These wounds may be difficult to detect until they have progressed to the point of causing noticeable symptoms or becoming infected. Your podiatrist may treat DFUs by removing pressure from the wound using a cast, boot, special footwear, or an off-loading device. Sometimes debriding the area, which involves removing damaged tissue from the wound site, is necessary. Keeping the foot clean, dry, and well moisturized is suggested in order to promote healing and prevent future wounds from developing. For more information about diabetic foot ulcers, please consult with a podiatrist.
Diabetic foot ulcers (DFUs) are slow-healing wounds that often form on the feet of people who have diabetes. These wounds may be difficult to detect until they have progressed to the point of causing noticeable symptoms or becoming infected. Your podiatrist may treat DFUs by removing pressure from the wound using a cast, boot, special footwear, or an off-loading device. Sometimes debriding the area, which involves removing damaged tissue from the wound site, is necessary. Keeping the foot clean, dry, and well moisturized is suggested in order to promote healing and prevent future wounds from developing. For more information about diabetic foot ulcers, please consult with a podiatrist.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions please contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.