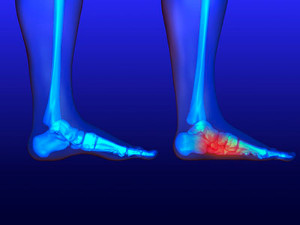
Causes and Treatment for Heel Pain

Heel pain, a common ailment, can be a source of discomfort that interferes with daily activities. The causes of heel pain can vary, with one of the most prevalent being plantar fasciitis. This condition involves inflammation of the plantar fascia, the thick band of tissue that supports the arch of the foot. Other common culprits include Achilles tendonitis, heel spurs, and bursitis. The good news is that heel pain is often treatable. Treatment options for heel pain range from conservative methods to more advanced interventions. Resting and performing gentle stretching exercises can provide relief, while custom-made orthotics may help distribute pressure more evenly. In severe or persistent cases, minimally invasive procedures such as corticosteroid injections may be recommended. Consulting a podiatrist is crucial in determining the underlying cause, in addition to guiding you toward the most suitable treatment plan. By addressing the root cause and following a tailored treatment regimen, you can take significant steps towards a pain-free and active lifestyle. It is strongly suggested that you visit a podiatrist who can accurately diagnose the cause for your heel pain and treat it accordingly.
Many people suffer from bouts of heel pain. For more information, contact one of our podiatrists of James Kutchback, DPM, CWS-P. Our doctors can provide the care you need to keep you pain-free and on your feet.
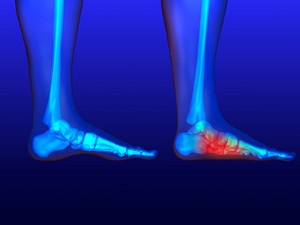
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Heel Pain
Have you ever gotten up from a chair or out of bed in the morning, and upon taking that first step, feel like your heel has stepped on a tack? Many people experience a feeling of sharp pain which radiates into their arch from their heel and which does not allow them to put their heel on the floor. Sometimes they need to sit back down, stand only on their toes and use the wall for balance. If you can take a few steps, it seems to go away and lessen, allowing you to then resume your activity. Later, throughout your day and after a period of rest, it can happen again. If this sounds familiar you may be suffering from your first attack of heel pain.
Heel pain is a debilitating condition that affects day to day activities. Running and walking both causes stress on the heel because the heel is the part of the foot that hits the ground first. This means that the heel is taking on your entire weight. Diagnosis and treatments for heel pain can be easily found through your podiatrist.
Plantar Fasciitis
One of the main causes of heel pain is a condition known as plantar fasciitis. The plantar fascia is a band of tissue that extends along the bottom of the foot, from the toe to the bottom of the heel. A rip or tear in this ligament can cause inflammation of these tissues, resulting in heel pain. People who do not wear proper fitting shoes are often at risk of developing problems such as plantar fasciitis. Unnecessary stress from ill-fitting shoes, weight change, excessive running, and wearing non-supportive shoes on hard surfaces are all causes of plantar fasciitis.
Achilles Tendonitis
Achilles tendonitis is another cause of heel pain. Similar to plantar fasciitis, inflammation of the Achilles tendon will cause heel pain due to stress fractures and muscle tearing. A lack of flexibility of the ankle and heel is an indicator of Achilles tendonitis. If left untreated, this condition can lead to plantar fasciitis and cause even more pain on your heel.
Heel Spur
A third cause of heel pain is a heel spur. A heel spur occurs when the tissues of the plantar fascia undergo a great deal of stress, leading to a separation of the ligament from the heel bone entirely. This results in a pointed fragment of bone on the ball of the foot, known as a heel spur.
Running With Flat Feet
Running is a pursuit that empowers both body and mind, regardless of foot arch type. Flat feet, often misunderstood, should not deter anyone from lacing up and hitting the track. There are various types of flat feet, each requiring a unique approach. Flexible flat feet involve arches that appear when one is off the foot, and rigid flat feet exhibit little to no arch, even when lifted. While some flat feet do not pose issues, others may lead to discomfort or pain during running. Wearing customized footwear with proper arch support is essential. Orthotics or insoles can aid in maintaining alignment and reducing strain. Performing strengthening exercises targeting foot muscles can enhance stability. Running with flat feet is indeed possible with the right knowledge, care, and preparation. If you have flat feet and are interested in pursuing running as a hobby, it is suggested that you are under the care of a podiatrist who can provide you with useful information.
Flatfoot is a condition many people suffer from. If you have flat feet, contact one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Flat Feet
Flatfoot is a condition that occurs when the arches on the foot are flattened, which allows the soles of the feet to touch the floor. Flatfoot is a common condition and it is usually painless.
Throughout childhood, most people begin to develop arches in their feet, however, some do not. Those who do not develop arches are left with flatfoot. The pain associated with flat feet is usually at its worse when engaging in activity. Another symptom that may occur with those who have this condition is swelling along the inside of the ankle.
It is also possible to have flexible flatfoot. Flexible flatfoot occurs when the arch is visible while sitting or standing on the tiptoes, but it disappears when standing. People who have flexible flatfoot are often children and most outgrow it without any problems.
There are some risk factors that may make you more likely to develop flatfoot. Those who have diabetes and rheumatoid arthritis have an increased risk of flatfoot development. Other factors include aging and obesity.
Diagnosis for flat feet is usually done by a series of tests by your podiatrist. Your podiatrist will typically try an x-ray, CT scan, ultrasound, or MRI on the feet. Treatment is usually not necessary for flat foot unless it causes pain. However, therapy is often used for those who experience pain in their flat feet. Some other suggested treatment options are arch supports, stretching exercises, and supportive shoes.
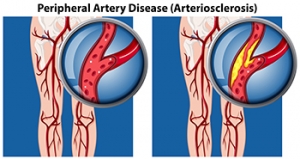
How Peripheral Artery Disease Can Affect the Feet
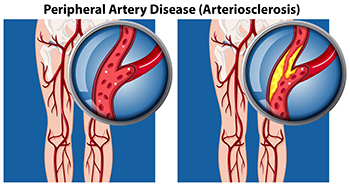
Peripheral artery disease, abbreviated PAD, also referred to as peripheral vascular disease, is a condition that arises from the reduced flow of blood to the body’s extremities, including the lower legs and feet. People with diabetes are more susceptible to developing PAD, as a result of weakened and damaged blood vessels from having high blood sugar. Blood clot formation within the vessels can also contribute to this condition. Conditions such as arthritis, which causes inflammation of the arteries, can further fuel peripheral artery disease. Other factors, such as smoking, hypertension, and obesity, increase the risk of developing PAD. Symptoms can include intermittent pain, coldness, numbness, and a bluish hue in the skin. In more advanced stages, wounds that resist healing, and areas of skin that blacken may develop due to the lack of adequate blood flow. In such cases, swift medical intervention is extremely important. If you suspect you may have peripheral artery disease that is affecting your lower extremities, it is suggested that you make an appointment with a podiatrist, who is specifically trained to manage this condition.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Lyme Disease and the Feet

Lyme disease, often transmitted by ticks, can bring about various symptoms that affect the feet and other parts of the body. While fever, fatigue, and rashes may signal its presence, a definitive diagnosis requires careful consideration of symptoms and circumstances. If one has been in wooded or grassy areas during tick season, it is possible to contract Lyme disease. Lyme disease's early signs, such as fever, chills, headache, fatigue, and muscle pain, can mimic a severe cold. Knee swelling is common, and joint pain may migrate across the body. As the disease progresses, headaches, Bell's palsy, and joint pain can intensify, and rare complications like heart involvement or mental health issues may arise. Shooting pains, numbness, or tingling in the hands and feet may be felt. It is suggested that you manage pain and inflammation and focus on your overall well-being to aid in healing. If you suspect you have Lyme disease, it is suggested that you make an appointment with a podiatrist for an accurate diagnosis and effective management.
When dealing with systemic disease of the feet, it is extremely important to check the affected areas routinely so that any additional problems are caught quickly. If you have any concerns about your feet and ankles contact one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors will assist you with all of your podiatric needs.
Systemic Diseases of the Feet
Systemic diseases affect the whole body, and symptoms usually are displayed in the feet. This condition can make a patient’s ability to walk unbearable. Systemic diseases include gout, diabetes mellitus, neurological disorders, and arthritis.
Gout – is caused by an excess of uric acid in the body. Common symptoms include pain, inflammation, and redness at the metatarsal/phalangeal joint of the base big toe. Gout can be treated by NSAIDs to relieve pain and inflammation, and other drugs that lower the acid levels in the body.
Diabetes mellitus – is an increase in the level of blood sugar that the body cannot counteract with its own insulin. Failure to produce enough insulin is a factor in Diabetes.
Diabetes of the Feet
Diabetic Neuropathy – may lead to damaged nerves and affect the feet through numbness and loss of sensation.
Peripheral Vascular Disease – can restrict the blood flow to the feet, and often times lead to amputation of the feet.
If you have any questions please contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Systemic Diseases of the Foot
There are several systemic diseases, or diseases that affect the whole body, that either display symptoms in the feet or affect the health of the feet. Common systemic diseases that affect the overall health of the feet, and the patient’s ability to walk comfortably, include gout, diabetes mellitus, neurological disorders, and arthritis, among others.
In gout, which is caused by an excessive buildup of uric acid in the body, the most common symptoms of pain, inflammation, and redness occur at the metatarsal/phalangeal joint at the base of the big toe. Any excess levels of uric acid crystallize and are deposited in tendons, joints, and surrounding bone and muscle tissue. Gout is commonly treated with NSAIDs to relieve pain and inflammation and other drugs to lower uric acid levels in the body. Gout most commonly affects those who are overweight, have low protein diets and lead a more sedentary lifestyle.
Diabetes mellitus is an increase in the level of blood sugar in which the body cannot counteract with naturally occurring insulin in the body. The three types of diabetes, Type I, Type II and Gestational Diabetes, are all signs the body is either not producing enough insulin or is not efficiently using the insulin that is produced. Gestational diabetes only affects women who are pregnant and have never, prior to pregnancy, exhibited symptoms of the disease.
There are two main issues that affect the feet that are commonly caused by diabetes. They include diabetic neuropathy and peripheral vascular disease. Diabetic neuropathy can lead to damaged nerves and affect the feet through numbness and loss of sensation. Peripheral vascular disease restricts the flow of blood to the foot and can, in extreme cases, lead to the necessity of amputating the foot. Peripheral issues that are caused by diabetes and can affect the foot include athlete’s foot, nail infections, corns, blisters, bunions, severe dry skin, plantar warts and ingrown toenails. These can all be attributed to the decrease of blood flow to the foot.
Neurological disorders and rheumatoid arthritis can also have severe impact on the health of the feet. Neurological disorders can affect the nerves in the main structure of the foot and cause loss of sensation and possible decreased muscle response. Rheumatoid arthritis can affect the bones and joint structures of the foot, making it impossible to walk normally without serious pain.
All systemic diseases that affect the foot can effectively be treated to minimize joint and muscle damage if they are diagnosed early and treated with medication and lifestyle therapy. Diabetes patients must monitor their blood sugar levels and work with their physician to keep their levels as close to normal as possible. Rheumatoid arthritis patients should work with their physician to ensure the proper medications are being taken to reduce the amount of damage to the joints of the body.
What Are the Causes and Treatments for Plantar Fasciitis?

Plantar fasciitis is a common foot condition that causes pain in the heel and bottom of the foot. The hallmark symptom is sharp, stabbing pain that is often most noticeable in the morning or after periods of inactivity. Plantar fasciitis occurs when the thick band of tissue that connects the heel bone to the toes, known as the plantar fascia, becomes inflamed or irritated. Several factors can contribute to plantar fasciitis, including overuse, high-impact activities, flat feet, and wearing improper footwear. Treatment typically involves a combination of rest, stretching exercises, physical therapy, and the use of supportive footwear or orthotic inserts. In severe cases, corticosteroid injections or extracorporeal shock wave therapy may be considered. To prevent plantar fasciitis, it is beneficial to maintain a healthy weight, wear appropriate shoes, and avoid excessive high-impact activities. Additionally, it can help to stretch regularly to keep the plantar fascia and surrounding muscles flexible and strong. Early intervention and diligent preventive measures can help alleviate the pain and discomfort associated with plantar fasciitis and promote better foot health. If you have plantar fasciitis, it is strongly suggested that you confer with a podiatrist who can offer treatment options that are best for you.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from James Kutchback, DPM, CWS-P. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.