The Woodlands
Woodville(936) 273-3311
Items filtered by date: August 2023
How Peripheral Artery Disease Can Affect the Feet
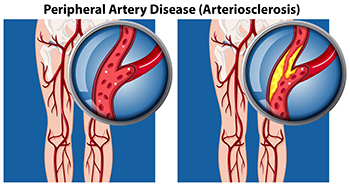
Peripheral artery disease, abbreviated PAD, also referred to as peripheral vascular disease, is a condition that arises from the reduced flow of blood to the body’s extremities, including the lower legs and feet. People with diabetes are more susceptible to developing PAD, as a result of weakened and damaged blood vessels from having high blood sugar. Blood clot formation within the vessels can also contribute to this condition. Conditions such as arthritis, which causes inflammation of the arteries, can further fuel peripheral artery disease. Other factors, such as smoking, hypertension, and obesity, increase the risk of developing PAD. Symptoms can include intermittent pain, coldness, numbness, and a bluish hue in the skin. In more advanced stages, wounds that resist healing, and areas of skin that blacken may develop due to the lack of adequate blood flow. In such cases, swift medical intervention is extremely important. If you suspect you may have peripheral artery disease that is affecting your lower extremities, it is suggested that you make an appointment with a podiatrist, who is specifically trained to manage this condition.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Dr. James Kutchback from James Kutchback, DPM, ABLES, CWS-P. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Lyme Disease and the Feet

Lyme disease, often transmitted by ticks, can bring about various symptoms that affect the feet and other parts of the body. While fever, fatigue, and rashes may signal its presence, a definitive diagnosis requires careful consideration of symptoms and circumstances. If one has been in wooded or grassy areas during tick season, it is possible to contract Lyme disease. Lyme disease's early signs, such as fever, chills, headache, fatigue, and muscle pain, can mimic a severe cold. Knee swelling is common, and joint pain may migrate across the body. As the disease progresses, headaches, Bell's palsy, and joint pain can intensify, and rare complications like heart involvement or mental health issues may arise. Shooting pains, numbness, or tingling in the hands and feet may be felt. It is suggested that you manage pain and inflammation and focus on your overall well-being to aid in healing. If you suspect you have Lyme disease, it is suggested that you make an appointment with a podiatrist for an accurate diagnosis and effective management.
When dealing with systemic disease of the feet, it is extremely important to check the affected areas routinely so that any additional problems are caught quickly. If you have any concerns about your feet and ankles contact Dr. James Kutchback from James Kutchback, DPM, ABLES, CWS-P. Our doctor will assist you with all of your podiatric needs.
Systemic Diseases of the Feet
Systemic diseases affect the whole body, and symptoms usually are displayed in the feet. This condition can make a patient’s ability to walk unbearable. Systemic diseases include gout, diabetes mellitus, neurological disorders, and arthritis.
Gout – is caused by an excess of uric acid in the body. Common symptoms include pain, inflammation, and redness at the metatarsal/phalangeal joint of the base big toe. Gout can be treated by NSAIDs to relieve pain and inflammation, and other drugs that lower the acid levels in the body.
Diabetes mellitus – is an increase in the level of blood sugar that the body cannot counteract with its own insulin. Failure to produce enough insulin is a factor in Diabetes.
Diabetes of the Feet
Diabetic Neuropathy – may lead to damaged nerves and affect the feet through numbness and loss of sensation.
Peripheral Vascular Disease – can restrict the blood flow to the feet, and often times lead to amputation of the feet.
If you have any questions please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What Are the Causes and Treatments for Plantar Fasciitis?

Plantar fasciitis is a common foot condition that causes pain in the heel and bottom of the foot. The hallmark symptom is sharp, stabbing pain that is often most noticeable in the morning or after periods of inactivity. Plantar fasciitis occurs when the thick band of tissue that connects the heel bone to the toes, known as the plantar fascia, becomes inflamed or irritated. Several factors can contribute to plantar fasciitis, including overuse, high-impact activities, flat feet, and wearing improper footwear. Treatment typically involves a combination of rest, stretching exercises, physical therapy, and the use of supportive footwear or orthotic inserts. In severe cases, corticosteroid injections or extracorporeal shock wave therapy may be considered. To prevent plantar fasciitis, it is beneficial to maintain a healthy weight, wear appropriate shoes, and avoid excessive high-impact activities. Additionally, it can help to stretch regularly to keep the plantar fascia and surrounding muscles flexible and strong. Early intervention and diligent preventive measures can help alleviate the pain and discomfort associated with plantar fasciitis and promote better foot health. If you have plantar fasciitis, it is strongly suggested that you confer with a podiatrist who can offer treatment options that are best for you.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. James Kutchback from James Kutchback, DPM, ABLES, CWS-P. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Why the Feet Swell During Pregnancy

During pregnancy, many women experience a condition known as edema. This swelling occurs in various parts of the body, including the feet, especially during the second and third trimesters. An increase of fluids in the lower part of the body may be the cause of swelling during pregnancy. The fluid gathers more at the end of the day, especially after standing for long periods. As the pregnancy continues, the uterus puts more pressure on the legs, ankles, and feet. The increased pressure can slow circulation, making it more difficult to return blood to the heart. Lying or sleeping on the back only increases the problem, especially in the third trimester. Some ways to combat the swelling include gentle exercise, reducing salt intake, wearing compression socks, and drinking more water. Walking and swimming are mild exercises that can be performed. While edema is considered normal during pregnancy, if discomfort from swelling in the feet increases, it is suggested that you seek attention from a podiatrist for guidance.
Pregnant women with swollen feet can be treated with a variety of different methods that are readily available. For more information about other cures for swollen feet during pregnancy, consult with Dr. James Kutchback from James Kutchback, DPM, ABLES, CWS-P. Our doctor will attend to all of your foot and ankle needs.
What Foot Problems Can Arise During Pregnancy?
One problem that can occur is overpronation, which occurs when the arch of the foot flattens and tends to roll inward. This can cause pain and discomfort in your heels while you’re walking or even just standing up, trying to support your baby.
Another problem is edema, or swelling in the extremities. This often affects the feet during pregnancy but tends to occur in the later stages.
How Can I Keep My Feet Healthy During Pregnancy?
- Wearing orthotics can provide extra support for the feet and help distribute weight evenly
- Minimize the amount of time spent walking barefoot
- Wear shoes with good arch support
- Wear shoes that allow for good circulation to the feet
- Elevate feet if you experience swelling
- Massage your feet
- Get regular, light exercise, such as walking, to promote blood circulation to the feet
If you have any questions please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Falling May Be Prevented

The percentage of people who are 65 years of age or older that fall every year is staggering. Research has shown approximately 20 percent of these falls can result in a serious injury, including broken ankles and toes. Many injuries can be avoided when effective fall prevention methods are implemented. These can include improving lighting in the household, and removing worn rugs from the living area. Many people choose to install grab bars in the shower and toilet area, in addition to using a non-slip bath mat. It is beneficial to have routine physical and eye examinations performed, and this is helpful in monitoring existing eyeglasses and medications. The body can become stronger with regular stretches practiced, which can be successful in preventing falling. If you would like more information about effective fall prevention techniques, it is suggested that you consult with a podiatrist who can provide you with the knowledge you are seeking.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Dr. James Kutchback from James Kutchback, DPM, ABLES, CWS-P. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our offices located in The Woodlands and Woodville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.



